What is diabetes?
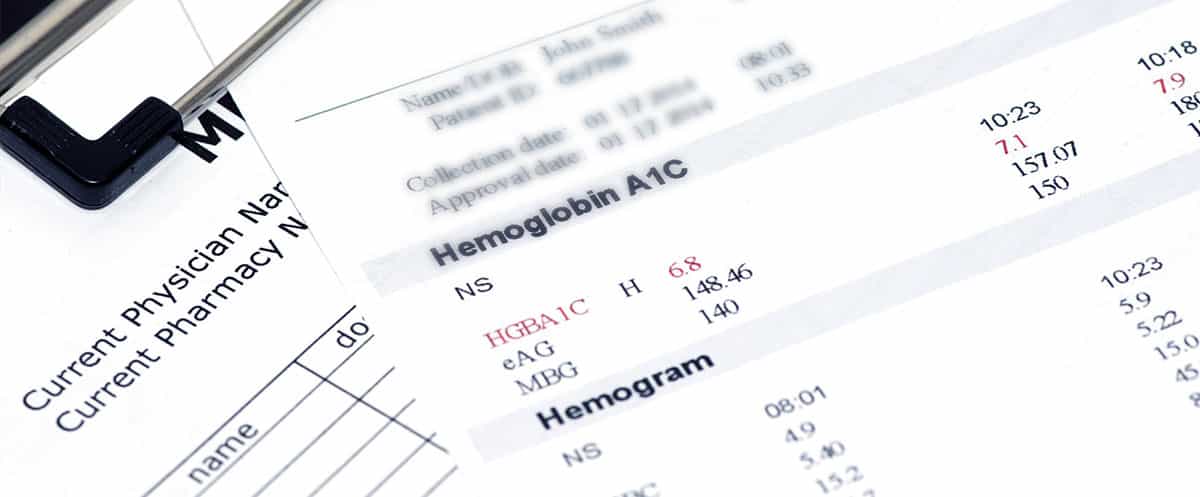
Diabetes is a chronic (long‐lasting) condition that occurs when the body cannot produce enough insulin or cannot effectively use the insulin it does produce. Insulin is a hormone produced in the pancreas that is needed to move glucose (sugar) from the blood into the body’s cells, where it is used for energy(fuel). When insulin is missing or not working properly, glucose levels in the blood rise. Diabetes is diagnosed when blood tests show elevated levels of glucose in the blood. Individuals can have diabetes for long periods of time without having any symptoms so it's important to know your risks and get screening tests to detect early disease.
If left undiagnosed or untreated, over time, the high blood glucose levels (known as hyperglycemia) can cause damage to many tissues in the body that may lead to disabling or life‐threatening health complications.
Type 1 diabetes
In type 1 diabetes, the body’s immune system attacks the insulin‐producing cells in the pancreas. As a result, the body can no longer produce enough insulin. It is not fully known or understood why this occurs. There appear to be genetic and probably environmental factors and the causes most likely differ from one individual to the next. Type 1 diabetes can affect people of any age, but it is usually first diagnosed during childhood or young adulthood.
People with this form of diabetes need insulin every day to manage the levels of glucose in their blood since they have severe or total insulin deficiency and insulin is needed to sustain healthy life. With daily insulin treatment, regular blood glucose monitoring, healthy eating and maintaining healthy lifestyles, people with type 1 diabetes can lead full and healthy lives.
Type 2 diabetes
Type 2 diabetes is the most common type of diabetes. It is seen most often in adults but can also be diagnosed in children and adolescents.In type 2 diabetes, the body can produce some insulin but is resistant to its effects. When this first starts, the body produces extra insulin to overcome the resistance, but over time, insulin production falls and insulin levels may become too low to be effective. This combination of insulin resistance and low insulin levels eventually leads to high levels of glucose in the bloodstream.
Unlike people with type 1 diabetes, people with type 2 diabetes may not require daily insulin treatment to survive. The essential treatments for type 2 diabetes include adopting a healthy eating plan, increasing physical activity, managing body weight and taking diabetes medicines and insulin as needed. Several pills and tablets as well as injectable therapies, including insulin, are available to help manage blood glucose levels for people with type 2 diabetes. Type 2 diabetes is usually a progressive disease (gets worse over time), which, if left untreated, can lead to many serious complications.If optimally managed however many people can also enjoy full, normal lives, which is the goal of therapy and monitoring.
Gestational diabetes
Gestational diabetes is a type of diabetes that is first detected during pregnancy and isn’t pre‐existing type 1 or type 2 diabetes. Gestational diabetes usually does not develop until the second or third trimester of pregnancy.In 2021, the International Diabetes Federation (IDF) estimated that 21.1 million births worldwide were affected by hyperglycemia. Of these, 80% were due to gestational diabetes.
Monitoring blood glucose levels and carefully following your doctor’s care plan will help keep you and your baby safe from complications related to gestational diabetes. Gestational diabetes usually goes away after pregnancy. However, if you've had gestational diabetes, you have a higher chance of getting it again in future pregnancies. Many women who have gestational diabetes go on to develop type 2 diabetes later in life. However, prevention is possible.
If you have been told you are at risk for diabetes or if you have prediabetes, making some lifestyle changes now can help you avoid or delay the onset of type 2 diabetes and other health complications, such as heart disease, down the road.
Remember to work with your healthcare team and follow the recommended guidelines on health screenings, healthy eating, exercising, and maintaining a healthy weight. It’s never too late to start. If you’ve been told by your doctor that you have prediabetes, be sure to get tested for diabetes as your healthcare provider recommends. Also, follow the recommended guidelines to help prevent type 2 diabetes. These include maintaining a healthy weight, exercising, healthy eating, reducing stress and even improving sleep. Taking care of diabetes includes a team of professionals with you at the center.
Sources:
IDF Diabetes Atlas, 10th edn. Brussels, Belgium: 2021. Last accessed online December 19, 2021.
International Diabetes Federation (IDF). What Is Diabetes. Last accessed July 7, 2022.
American Diabetes Association (ADA). Gestational Diabetes : Treatment & Perspective.Last accessed online June 23, 2022
US-VRF-1900008