The Signs and Symptoms of Diabetes
By: Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, FADCES
The hallmark of all forms of diabetes is high blood sugar, also called hyperglycemia. This can cause several symptoms, including:
- Increased urination
- Hunger
- Tiredness
- Feeling thirsty
- Blurry vision
- Dry skin
- Weight loss
- Numb or tingling hands
- Infections

Before we dive deeper into the signs and symptoms of the different types of diabetes, let’s do a high-level review of the condition.
What Is Diabetes?
Diabetes is a condition in which there is not enough insulin to meet the body’s needs, either because the body is not making insulin or it is not using the insulin it makes as well as it should. Insulin can be thought of as the key that unlocks the doors of the cells to let glucose (sugar) into the cells for use as energy. Without insulin, the cells do not get enough energy, and too much glucose stays in the blood stream, where it can cause serious health problems over time.
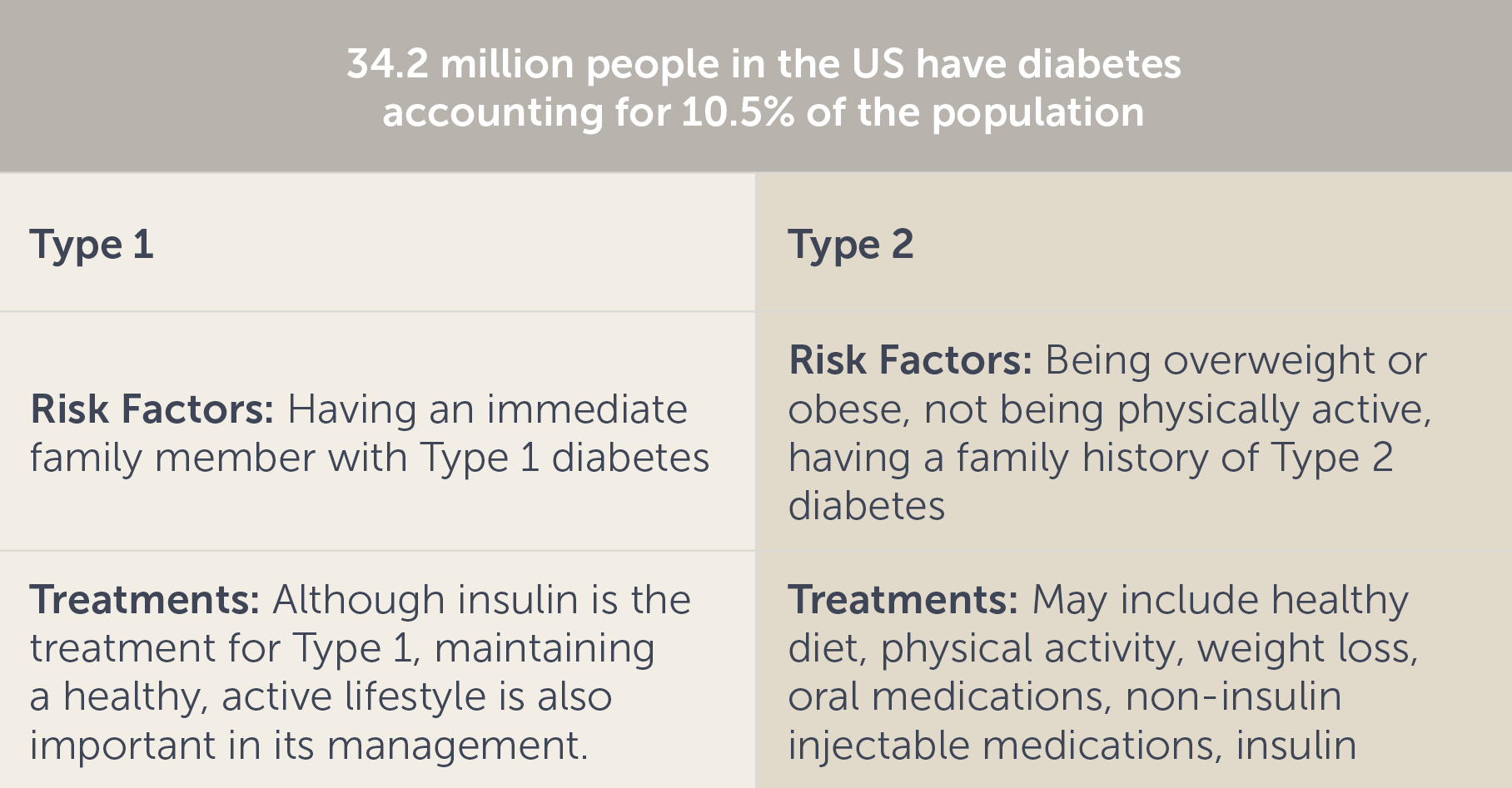
There are three main types of diabetes: Type 1, Type 2, and gestational diabetes.
Type 1 diabetes represents approximately 5%-10% of diabetes cases and is thought to be caused by an autoimmune response, in which the body’s immune system attacks its own insulin-producing cells in the pancreas. Because this leads to a lack of insulin, people with Type 1 diabetes require insulin treatments.
Risk factors for Type 1 diabetes are not as clear as they are for Type 2 diabetes, but there are some known risk factors such as family history (having a parent, brother, or sister with Type 1 diabetes) and age. Although it can develop at any age, Type 1 diabetes most commonly develops when you’re a child, teen, or young adult. Currently, no one knows how to prevent Type 1 diabetes.
Type 2 diabetes accounts for 90%-95% of diabetes cases and is the result of abnormal functioning in many different body systems. A major feature of Type 2 diabetes is insulin resistance, which means the body produces insulin – and sometimes even extra insulin – but the cells of the body do not respond normally to it. People with Type 2 diabetes can often be treated with oral medications or non-insulin injectable medications, in addition to a healthy diet and physical activity. Sometimes, people with Type 2 diabetes need insulin treatments.
Type 2 diabetes occurs most often in adults, and risk increases with age; however, a rise in overweight and obese children has led to more cases of Type 2 diabetes in younger age groups.
You’re at risk for developing Type 2 diabetes if you:
- Are overweight
- Are 45 years or older
- Have a parent, brother, or sister with Type 2 diabetes
- Are physically active less than 3 times a week
If you have non-alcoholic fatty liver disease you may also be at risk for Type 2 diabetes.
Type 2 diabetes can be prevented with simple lifestyle changes such as losing weight if you’re overweight, eating healthier, and getting regular physical activity.
Gestational diabetes is diabetes that typically develops in the second trimester of pregnancy. After delivery of the baby, glucose levels usually return to normal. Women who had gestational diabetes have a higher risk of developing Type 2 diabetes later in life.
In addition to the three main types of diabetes, there is also prediabetes. Prediabetes is when glucose is higher than it should be but doesn’t quite meet the diagnosis of diabetes. People with Type 2 diabetes often first experience prediabetes. Prediabetes doesn’t typically cause any symptoms, but indicates a very high risk of developing Type 2 diabetes. Over eighty-eight million adults in the US have prediabetes, and more than 8 out of 10 do not know that they have it. It’s estimated that 15%-30% of people with prediabetes could develop Type 2 diabetes within 5 years if they take no action.
Signs and Symptoms of Diabetes
The types of diabetes evolve and present differently. Type 2 diabetes develops slowly, and a person may not be diagnosed until they’ve had the disease for a long time. Gestational diabetes, which is often without signs and symptoms, is usually discovered through a routine lab test performed during pregnancy. Type 1 diabetes can develop quickly, within weeks or months. In addition to experiencing the symptoms mentioned earlier, people with Type 1 (and some with Type 2) diabetes can develop a very serious condition called diabetic ketoacidosis (DKA). This occurs when the body does not have enough insulin to allow glucose into the cells for use as energy. The body uses fat for energy instead, which creates ketones and acids. When too many ketones and acids build up, they can be life-threatening. The symptoms of DKA include extreme thirst, nausea, stomach pain, fruity-smelling breath, and difficulty breathing, in addition to symptoms of hyperglycemia.
Risk factors for Diabetes
One big risk factor for Type 1 diabetes is having an immediate family member with Type 1 diabetes. The risk for developing prediabetes or Type 2 diabetes increases with age, in addition, being overweight or obese, and a lack of physical activity can increase the risk. Certain groups of people have a higher risk of developing Type 2 diabetes, including African Americans, Hispanics/Latinos, American Indians, Alaska Natives, and Native Hawaiians and Pacific Islanders.
The risk factors for gestational diabetes are similar to those for Type 2 diabetes. Having had gestational diabetes or a large baby (weighing more than 9 pounds) during a previous pregnancy and having polycystic ovary syndrome (PCOS) are additional risk factors.
Is Diabetes Preventable?
Intensive lifestyle interventions have been shown to help prevent or delay Type 2 diabetes. The Diabetes Prevention Program (DPP) is a structured program focused on healthy eating, a goal of a 7% or greater weight loss and 150 minutes of moderate-intensity physical activity per week. The DPP demonstrated that an intensive lifestyle therapy intervention could reduce the incidence of Type 2 diabetes by 58% over 3 years in people with prediabetes. Type 2 diabetes is considered a chronic condition. Lifestyle changes such as weight loss, physical activity, and moderating carbohydrate intake, along with diabetes self-management education and support, have the potential to help manage the condition.
When to See a Doctor
Every person with diabetes should have a doctor and schedule regular check-ups at least every 3 to 6 months. In addition to check-ups, you should contact your doctor when your blood sugars are consistently above or below targets. If you are not sure of your targets, be sure to ask your doctor.
At your doctor’s appointment, have any recent labs ready to discuss, especially if they were done at a location outside of your health system. Bring your paper glucose log book and any diabetes-related devices that you use, such as your blood glucose meter or CGM, as well as any information you may store in mobile apps such as digital glucose logs and food logs. It’s also helpful to bring an up-to-date medication list or your medication bottles for a full review. Below is a list of helpful questions about diabetes to consider asking your doctor or diabetes care team:
- Is my A1C at goal?
- What are my glucose targets?
- What percent of my glucose readings are in range and how can I improve it?
- How often should I monitor my glucose?
- How should I treat a high or low glucose level?
- Are there any new medications or technologies that can help me better manage my diabetes?
- Is there a certain type of diabetes meal plan I should follow?
- How often should I exercise?
- How do my diabetes medications work?
- Am I on any other medications that may affect my glucose levels or weight?
- Are there any apps, websites, or peer support groups that you recommend?
Each person with diabetes should have a healthcare team supporting them. Meet with a diabetes care and education specialist who can answer questions, direct you to classes and connect you with resources such as pharmacists, exercise physiologists, social workers, dieticians, and psychologists.
Sources:
Cleveland Clinic. Hyperglycemia (High Blood Sugar). Accessed July 26, 2021.
Centers for Disease Control and Prevention. Accessed July 26, 2021.
American Diabetes Association. 3. Prevention or delay of type 2 diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020;43(Suppl. 1):S32–S36 Accessed June 24, 2021.
American Diabetes Association. 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021;44(Suppl. 1):S53–S72
US-OTB-2100072








